Delirium Tremens (DTs) is a severe form of alcohol withdrawal that occurs in about 5% of those undergoing detoxification, as per the National Institute on Alcohol Abuse and Alcoholism (NIAAA). This condition can be life-threatening, with up to a 15% mortality rate without medical treatment. It typically arises after prolonged heavy alcohol use when drinking is suddenly stopped. Immediate medical intervention is critical to manage and mitigate the severe outcomes of DTs.
The primary cause of delirium tremens is the abrupt cessation of alcohol in individuals with physical dependency. Chronic drinking alters brain chemistry and leads to nervous system hyperactivity when alcohol is withdrawn. The risk of developing DTs increases with the duration and intensity of alcohol consumption and is exacerbated by previous withdrawal episodes or the use of other sedatives.
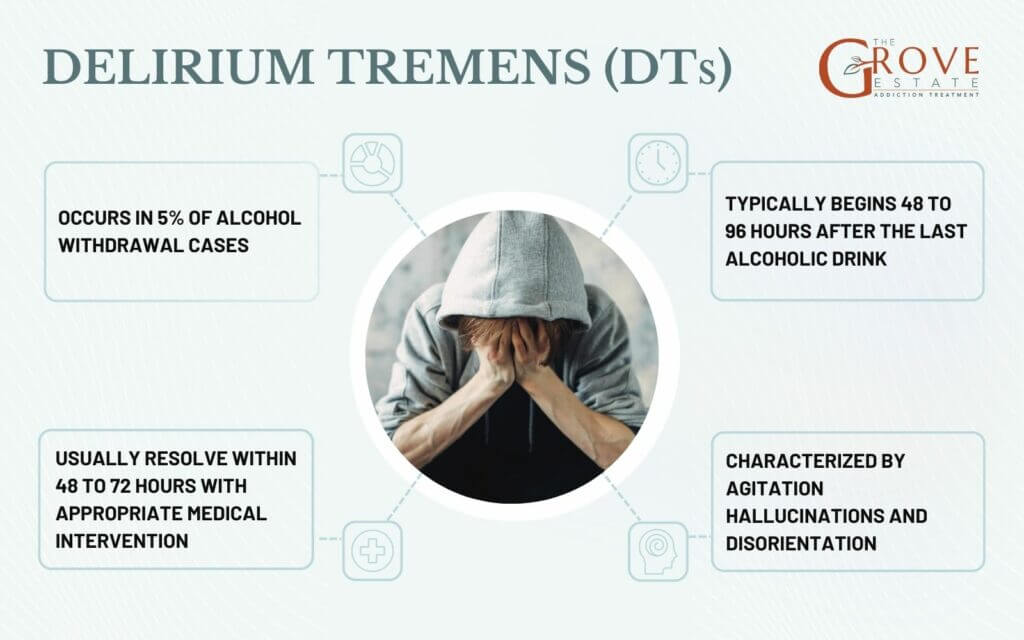
Symptoms of delirium tremens range from severe confusion and tremors to hallucinations. These symptoms usually appear within 48 to 96 hours after the last alcoholic drink, but they can be delayed up to 10 days. These symptoms can escalate rapidly, making it critical to seek urgent medical care to prevent worsening conditions.
Delirium tremens creates significant health risks like dehydration and seizures. These complications increase the risk of death, especially in older adults, those in poor health, or with a history of severe withdrawals. Early recognition and medical monitoring are essential to manage these risks effectively.
Treatment of delirium tremens must be carried out in a hospital setting and involves the use of benzodiazepines to control withdrawal symptoms, agitation, and prevent seizures. Supportive care includes fluid replacement, nutritional support, and vital signs monitoring. For severe cases, intensive care may be necessary to ensure patient stability and recovery.

What is Delirium Tremens?
Delirium Tremens (DTs) is a severe and acute condition that manifests as part of the alcohol withdrawal syndrome. It typically develops in individuals with a history of heavy and prolonged alcohol use who suddenly discontinue or decrease their alcohol intake. This condition is recognized medically as a life-threatening complication due to the dramatic chemical imbalance it causes in the brain, primarily affecting neurotransmitter systems that have been altered by chronic alcohol exposure. DTs is distinguished from other forms of alcohol withdrawal by its intensity and the serious risk it poses, necessitating prompt and effective medical treatment to prevent potentially fatal outcomes.
What Causes Delirium Tremens?
Delirium Tremens (DTs) is caused by a significant reduction in alcohol intake after prolonged periods of heavy drinking. The underlying mechanism involves the abrupt disruption of the central nervous system’s adaptation to the presence of alcohol. Chronic alcohol consumption affects neurotransmitter systems, notably gamma-aminobutyric acid (GABA) and glutamate. GABA is an inhibitory neurotransmitter, and alcohol enhances its effects, leading to a depressive effect on the brain. When alcohol is suddenly removed, the brain experiences a rebound or hyper-excitatory state due to the reduced inhibitory effects of GABA and increased activity of excitatory neurotransmitters like glutamate. This sudden shift leads to neurological and physiological disturbances manifesting as Delirium Tremens.
How Does Delirium Tremens Affect the Body?
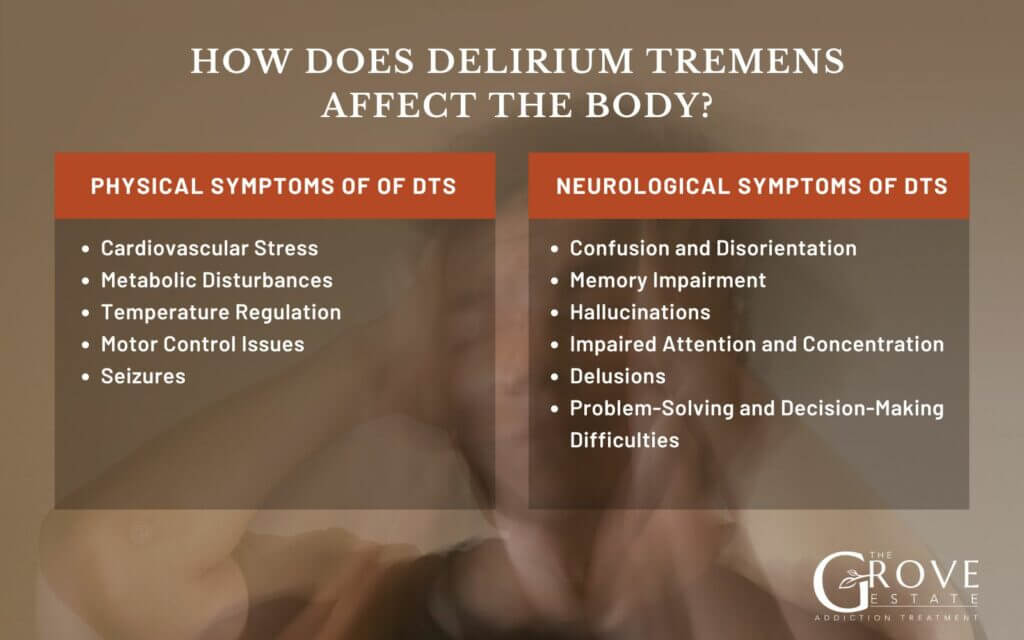
Delirium Tremens (DTs) significantly impacts the body both neurologically and physically. It is a critical condition that demands immediate medical attention to manage these diverse and potentially fatal effects on the body. Here are some key symptoms of Delirium Tremens:
Physical Symptoms of Delirium Tremens
- Cardiovascular Stress: The body’s stress response is heightened during DTs, leading to increased heart rate, blood pressure, and the risk of cardiac arrhythmias. These cardiovascular changes are responses to the sudden nervous system stimulation and can be life-threatening if not managed properly.
- Metabolic Disturbances: The withdrawal process can cause severe metabolic instability, including electrolyte imbalances and dehydration. These conditions arise from increased sweating, vomiting, and the potential for reduced fluid intake due to nausea and agitation.
- Temperature Regulation: DTs often cause fever and sweating as part of the body’s acute response to alcohol withdrawal. These symptoms reflect the central nervous system’s overactivity and the body’s attempt to regulate its internal environment under stress.
- Motor Control Issues: Tremors and muscle coordination problems are common, making even simple physical tasks challenging. These symptoms are due to the neurological disturbances affecting the motor areas of the brain.
- Seizures: One of the most dangerous effects of DTs is the potential for seizures, which occur due to the brain’s heightened electrical activity and instability during withdrawal.
Neurological Symptoms of DTs
- Confusion and Disorientation: One of the hallmark symptoms of DTs is a significant level of confusion. Individuals may have trouble understanding where they are, what time it is, or what is happening around them.
- Memory Impairment: Short-term memory loss is common, and individuals may have difficulty retaining new information.
- Hallucinations: Cognitive disturbances during DTs often include visual, auditory, or tactile hallucinations. Individuals may see or hear things that aren’t there, adding to their confusion and fear.
- Impaired Attention and Concentration: The ability to focus or maintain attention on tasks or conversations is severely compromised.
- Delusions: Some individuals may experience delusions, or false beliefs, that are often paranoid or persecutory in nature. This leads to agitation and unpredictable behaviors.
- Problem-Solving and Decision-Making Difficulties: The ability to think logically or make decisions can be impaired, leading to poor judgment and risky behaviors that might not occur if the individual were thinking clearly.
How is Delirium Tremens Diagnosed?
Delirium Tremens is diagnosed based on clinical evaluation, typically by a healthcare professional observing the specific symptoms and reviewing the patient’s drinking history. Key indicators include severe confusion, agitation, fever, hallucinations, and tremors. Medical professionals also consider vital signs like elevated heart rate and blood pressure, which often accompany DTs. Laboratory tests might be conducted to rule out other causes of symptoms and to check for complications like electrolyte imbalances and dehydration. A diagnosis of DTs requires urgent medical treatment due to its potentially life-threatening nature.

What are the Health Risks if Delirium Tremens Develops?
Delirium Tremens (DTs) carries several serious risks that can have immediate and long-term consequences:
- Mortality: One of the most severe risks associated with DTs is the high mortality rate. This risk is primarily due to the possibility of severe cardiovascular complications and seizures.
- Seizures: Seizures are a common and dangerous risk during DTs. They will lead to further complications, including injury during a seizure and the potential for status epilepticus, a life-threatening condition where the brain is in a state of persistent seizure.
- Cardiac Complications: The stress on the cardiovascular system can lead to serious issues such as arrhythmias, high blood pressure, and even heart failure, especially in individuals with pre-existing heart conditions.
- Dehydration and Metabolic Imbalance: Intense sweating, vomiting, and fever can lead to dehydration and significant electrolyte imbalances, which can affect critical body functions and contribute to the risk of seizures and heart problems.
- Psychiatric Problems: Beyond the immediate crisis, individuals who experience DTs may have long-term psychological issues, such as worsened mental health disorders, prolonged cognitive deficits, and an increased risk of future severe withdrawal episodes.
- Injury: During episodes of severe confusion and agitation, there is a heightened risk of accidental injury. This can include falls, collisions, or self-inflicted harm.
Given these risks, Delirium Tremens should be treated as a medical emergency, and individuals showing signs of severe alcohol withdrawal should receive prompt medical attention to manage and mitigate these risks effectively.
How is Alcohol Withdrawal Different From Delirium Tremens?
Alcohol withdrawal and Delirium Tremens (DTs) are related but distinct conditions within the spectrum of alcohol withdrawal symptoms. Delirium Tremens is a more severe and dangerous form of alcohol withdrawal that typically occurs in a small percentage of individuals undergoing withdrawal. While alcohol withdrawal is typically managed at home or with minimal medical intervention for many, DTs requires immediate hospitalization and intensive medical treatment due to the high risk of serious complications and death. While all cases of DTs are a form of alcohol withdrawal, not all alcohol withdrawal escalates to Delirium Tremens.
What is the Timeline for DTs?
Delirium Tremens typically begins 48 to 96 hours after the last alcoholic drink, but it can start as late as 10 days post-cessation. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), symptoms peak around the fourth to the fifth day and usually resolve within 48 to 72 hours with appropriate medical intervention. However, the duration can vary depending on factors such as the severity of the alcohol dependency and the individual’s general health. It’s important to note that up to 5% of individuals withdrawing from alcohol experience Delirium Tremens, highlighting its severity among withdrawal symptoms.

What are the Treatment Options for Delirium Tremens?
The treatment for Delirium Tremens primarily involves medical intervention in a controlled environment such as a hospital. The key is to stabilize the patient and manage symptoms effectively to prevent complications. Here are the main treatment options:
- Benzodiazepines: These are the first-line treatment for managing the symptoms of DTs, including agitation, tremors, and seizures. They help calm the nervous system and reduce withdrawal symptoms.
- Fluid Replacement and Nutritional Support: Due to the risk of dehydration and nutritional deficiencies, patients often require IV fluids and supplements, especially thiamine, to prevent complications such as Wernicke-Korsakoff syndrome.
- Antipsychotics: These are used to control severe hallucinations or agitation if benzodiazepines are insufficient.
- Monitoring and Supportive Care: Continuous monitoring of vital signs and mental status is critical to adjust treatments as needed and ensure the safety of the patient.
- Treatment of Concurrent Medical Issues: Addressing any co-existing medical conditions or complications that arise during withdrawal is crucial for recovery. Behavioral Therapy and Inpatient Treatment are necessary to recovery from alcoholism which can in turn prevent DT’s.
Where Can I Find Help for Delirium Tremens?
If you or someone you know is experiencing symptoms of Delirium Tremens, immediate medical attention is critical due to the severe and potentially life-threatening nature of the condition. The best course of action is to call emergency services or head to the nearest emergency room where urgent care can be provided. Delirium Tremens requires inpatient treatment in a hospital setting where medical professionals can closely monitor and manage withdrawal symptoms.
For ongoing support and management of alcohol dependency, addiction treatment centers offer specialized programs under medical supervision that include detoxification and rehabilitation. Consulting with a primary care physician will also help as they provide referrals to specialists in addiction medicine and mental health professionals. Psychiatrists and therapists who specialize in addiction will further assist in recovery by offering therapy and guidance, ensuring a comprehensive approach to treatment and prevention of future episodes.
Can Delirium Tremens (DTs) occur in individuals who are not chronic alcoholics?
Yes, DTs can also affect individuals experiencing sudden alcohol withdrawal after heavy drinking, known as “acute DTs,” even if they don’t have a long history of alcoholism.
Are there specific risk factors for severe DTs?
Yes, factors like previous DT episodes, older age, concurrent medical conditions (like liver disease), other substance dependencies, and abrupt alcohol cessation can increase the risk of severe DT symptoms.
Can DTs occur with medical alcohol withdrawal treatment?
While treatment reduces DT risk, it can still occur, especially with delayed or insufficient care. Individual responses and withdrawal progression also affect DT likelihood despite medical intervention.
What role does family support play in the recovery from delirium tremens?
Family support is crucial in the recovery process from Delirium Tremens and alcohol dependency in general. Effective recovery often involves a comprehensive support system that includes medical professionals and close family members. Families can provide the necessary emotional support and motivation needed for an individual to pursue and adhere to treatment plans. Furthermore, as outlined on WebMD, family members can also play a key role in recognizing early signs of alcohol withdrawal and ensuring that the individual receives the necessary medical attention promptly.
Incorporating family integration into the treatment and recovery plan can significantly enhance the effectiveness of the overall strategy. This integration helps maintain a stable environment, reduces the risk of relapse, and supports the psychological well-being of the recovering individual, thereby contributing to a more sustainable recovery from alcohol dependency and its severe withdrawal symptoms.
How do co-occurring mental health disorders impact the treatment of delirium tremens?
Co-occurring mental health disorders can significantly complicate the treatment of Delirium Tremens. Individuals with underlying psychiatric conditions such as anxiety, depression, or bipolar disorder may experience more severe withdrawal symptoms and are at a higher risk of developing DTs. According to WebMD, these disorders can exacerbate the stress of withdrawal, leading to more intense and challenging symptoms that require specialized medical attention.
Treatment strategies must therefore be adapted to address both the physical symptoms of DTs and the psychological aspects of co-occurring disorders. This dual approach ensures that all underlying issues are addressed, which is crucial for effective recovery. Medical professionals often recommend a holistic treatment plan that includes alcohol withdrawal delirium management and psychiatric care to provide comprehensive support to the patient.

Share This Post